HEMOCYTOMETRY
The technique of counting of the blood cells is known as hemocytometry . This involves manual counting of the cell with the help of a microscope after diluting blood in respective diluting fluids . The cells most often counted by this technique are red cells white cells platelets and eosinophils . The differentiate the various types of the individual cells .
Requirements
1 . Microscope

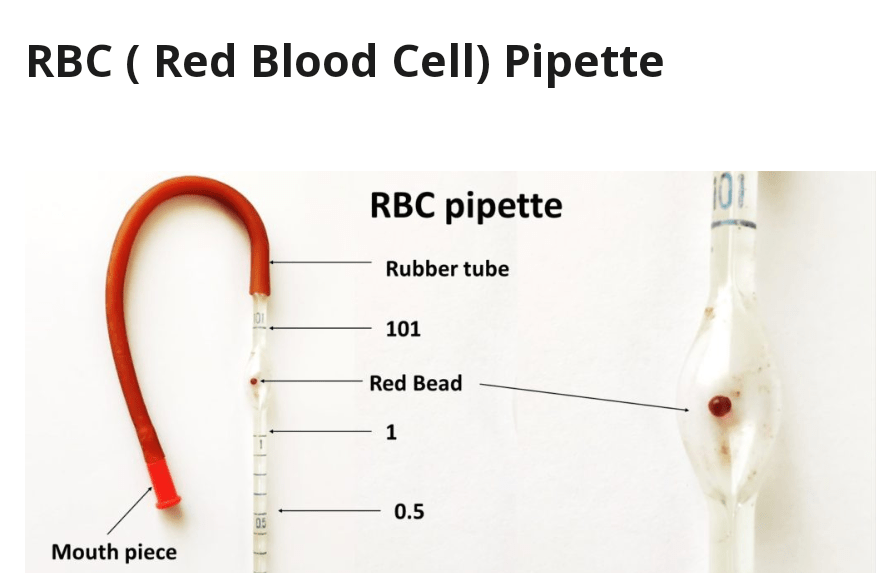
2 . RBC pipette
- This pipette has a large bulb which contains a red glass bead .
- It has three marks 0.5 , 1.0 and 101 .
- Blood is drawn to 0.5 mark and then diluting fluid is drawn up to the mark 101 .
- The diluting of blood is 1: 200 .
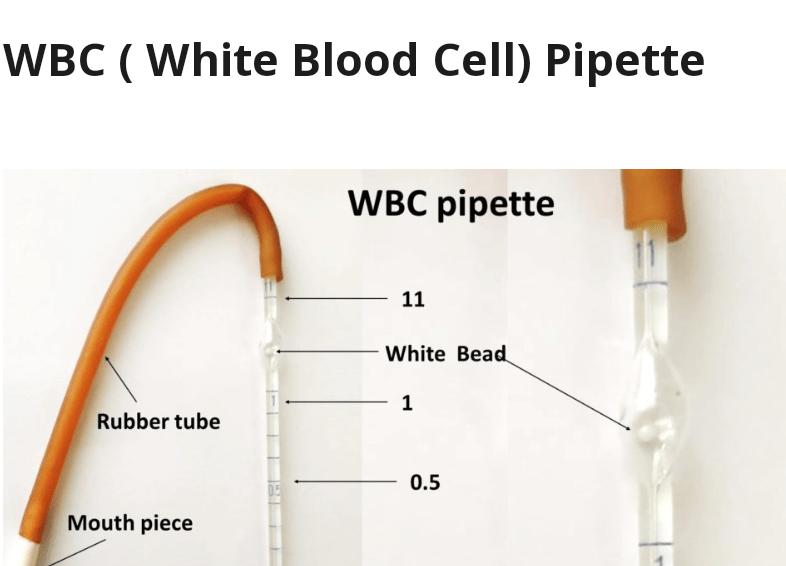
3 . WBC pipette
- It is smaller than the red cell pipette and it’s bulb contain a white glass bead .
- It has three marks 0.5 , 1.0 and 11 .
- The blood is drawn up to 0.5 mark and then diluting fluid is drawn up to 11 Mark
- The dilution of blood is 1 : 20 .
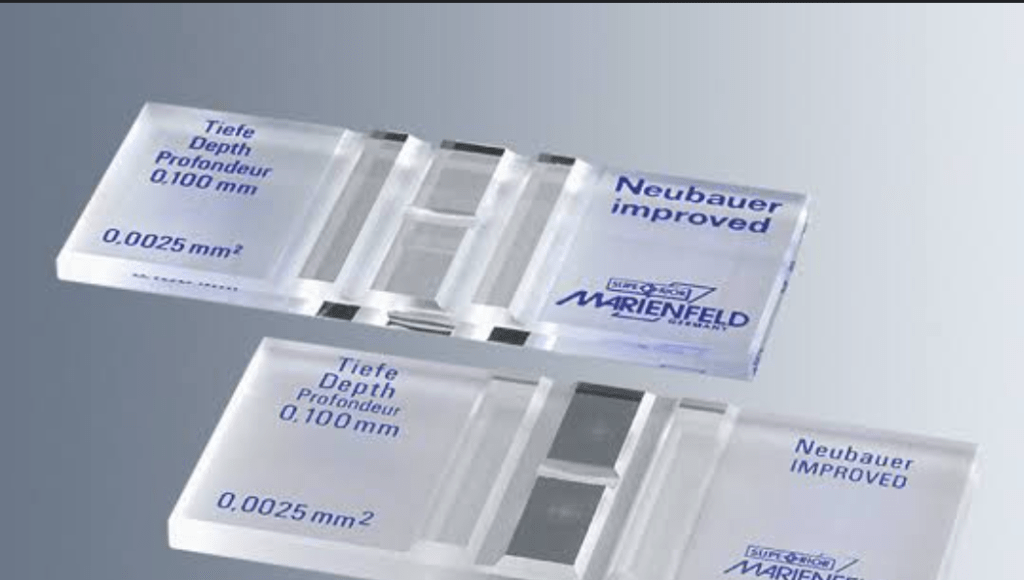
4 . The counting chamber
- The chamber most commonly used is the improved Neubauer chamber which has an area of 9 sq. mm and a depth of 0.1 mm .
- The two stages are separated from two ridges one on either side by a gutter .
- The surface of the two ridges is 1/10 mm above the stage .
- The 9 sq. mm area of the counting chamber is divided into 9 square . The four corner squares measure 1 sq. mm area .
- The central square is divided into 25 squares and each of these square measures 1/400 sq. mm in area .
- Five of the medium squares ( or 80 small squares ) are used in counting red cells .
5 . Cover slips
A special type of cover slip is used with a very smooth and even surface . These are available in two sizes
- 16 × 22 mm
- 22 × 23 mm .
The thickness of the cover slips may be 0.3 mm , 0.4 mm or 0.5 mm .
Total Red Blood Cells (RBC) Count
Total Red Blood Cells (RBC) Count Is important in diagnostic hematology . RBC count is useful to calculate MCV and MCH . The manual method of RBC count is time consuming and imprecise . The reference method preferred for RBC count is an automated method .
Clinical significance
At birth the total erythrocyte count varies from 6.5 millions to 7.25 millions per cubic mm ( Cumm ) . There is steady decline after a few hours and at the end of 15 days to one month there is a slow rise to normal adult levels .
An increase in total erythrocyte count is observed in conditions such as
- Hemoconcentration due to burns dehydration etc .
- In central cyanotic states as seen in chronic heart disease conditions of decreased lung functions such as emphysema and in polycythemia .
Decrease in erythocyte count is observed in
- Old age
- In pregnancy
- Anemias
Normal values
| Male | 4.5 to 6.0 million/Cumm |
| Female | 4.0 to 4.5 million/Cumm |
Specimen
1 . Double oxalate or EDTA blood
2. Capillary blood ( The specimen need not be a fasting sample )
Principle
The blood specimen is diluted 1:200 with the RBC diluting fluid and cell are counted under high power (40 × Objective ) by using a counting chamber . The number of cell in undiluted blood are calculated and reported as the number of red cells per Cumm (microlitter ) of whole blood .
Requirments
- Microscope
- Improved Neubauer chamber
- RBC pipette
- RBC diluting fluid ( Dacies fluid )
It is prepared as follows
| Sodium citrate | 3 . 0 g |
| Formalin | 1. 0 ml |
| Distilled water | 100 ml |
This solution is stable at room temperature ( 25° C +_ 5 ° C ) for at least one year .
Procedure
- Mix the anticoagulant blood carefully by swirling the bulb .
- In the case of capillary blood the lencet stab should be sufficiently deep to allow free of blood . It is drawn quickly in the RBC pipette .
- Draw blood up to 0.5 mark .
- Carefully wipe the excess blood outside the pipette by using cotton or a gauze .
- Draw diluting fluid up to 101 mark .
- The pipette is rotated by keeping it horizontal during mixing .
- After five minutes by discarding few drops from the pipette and holding it slightly inclined small volume of the fluid is introduced under the covers slip which is placed on the counting chamber .
- Allow the cells to settle for 2 to 3 minutes .
- Place the counting chamber on the stage of the microscope .
- Switch to low power ( 10 x ) objective . Adjust light and locate the large square in the center with 25 small squares .
- Now switch to high power ( 40 x ) objective .
- The red blood cells in the four corner squares and in the center square ( marked in the diagram as`
R` ) are counted . - Use following formulae for the calculation of red blood cells .
calculation
Total red blood cells per liter of blood = RBCs / Cumm ( microlitter ) × 10 ⁶
Additiinal information
For diluting of blood instead of using an RBC pipette following methodology is preferred
- By using a 20 microlitter ( standardized ) pipette 20 microlitter of blood is mixed with 4 ml of RBC diluting fluid in a glass test tube ( 10 × 75 mm ) . It mixed well and then small volume of this fluid is introduced into a counting chamber .
- The errors of blood counting by visual means are very considerable due to the random distribution of the cells in the counting chamber . The movement of the calls in the chamber during the fillings process causes them to collide and this influences their distribution . The inherent distribution error can be reduced by counting more cells .
- To confirm specific results it is better to repeat a count using a second chamber and pipette than to count double the number of cells in single fillings of the counting chamber .
Sources of Error
Falsely high red blood cells counts are obtained due to the following reasons
- Collection of blood from the area where there is hemoconcentration .
- Inadequate wiping of the pipette .
- Improper pipetting of the blood as well as the fluid .
- Improper mixing .
- Uneven distribution in the counting chamber .
- Error in calculations .
Falsely low red blood cell count are obtained due to the following reasons
- Blood dilution with tissue fluid due to edema or squeezing .
- Improper pipetting and dilution ( Where blood draw is less and if dilution is above the mark ) .
- Dilution of the contents in the pipette by saliva .
- Uneven distribution of the cells in the counting chamber .
- Error in calculations .
- Use of improperly standardized counting chamber and bad adjustment of cover slip .
- Due to partially clotted blood specimen .
