Differential Leukocyte count ( DLC )
Clinical Significance
Differential count is useful to identify changes in the distribution of white cells which may be related to specific types of disorders . It also gives idea regarding the severity of the disease and the degree of response of the body .
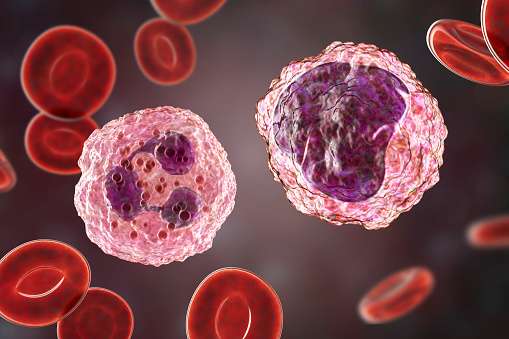
Neutrophils
Increase in the percentage of neutrophils is called neutrophilia . All the physiological causes that produce leukocytosis give rise to neutrophilia . The commonest pathological cause is pyogenic bacterial infection . Decrease in neutrophils ( Neutropenia ) is observed in infections such as bacterial ( Typhoid ) viral ( measles , influenza etc . ) and in other conditions such as Anemias ( Aplastic , Megaloblastic , iron deficiency ) and in suppression of bone marrow by various drugs and radiation .
Bleeding Time (BT) and Clotting Time (CT) Test
Lymphocytosis
It may be relative or absolute .
- Relative lymphocytosis
In this condition the actual number of lymphocytes is unchanged but due to decrease in neutrophils mainly the differential count shows an increase in lymphocyte .
- Absolute lymphocytosis
It is observed in the case of the following
1 . Children
2 . Certain infections such as mumps , cough , measles , influenza , syphilis, tuberculosis , typhoid and other chronic infections
3 . Infectious mononucleosis
4 . Chronic lymphocytic leukemia
- Lymphopenia
It is observed in acute stages of infections and in excess irradiation .
- Eosinophilia
It is observed in asthma , hypersensitivity reaction , parasitic infestations and in chronic inflammatory diseases .
- Monocytosis
It is observed in Tuberculosis , Malaria , Subacute Bacterial endocarditis , Typhoid and in Kala azar .
- Basophilia
It is usually observed in chronic myeloid leukemia .
Normal values ( Male or Female )
| Neutrophils 1 . Segmented 2 . Band forms | 40 – 75 % ( mean 57 % ) 2 – 6 % ( mean 3 % ) 50 – 70 % ( mean 54 % ) |
| Eosinophils | 1 – 4 % ( mean 2 % ) |
| Basophils | 0 – 1 % |
| Lymphocytes | 20 – 45 % ( mean 37 %) |
| Monocytes | 2 – 8 % ( mean 6 % ) |
Specimen
The blood smears should be preferable prepared immediately after skin puncture or venipuncture before mixing with anticoagulant . If EDTA blood is used the smears should be prepared within 1 to 2 hours after blood drawing . Other anticoagulants do not give satisfactory results . The blood smears should be immediately fixed in methanol .
Requirements
1 . Microscope slides and a glass spreader
2 . Cedar wood oil ( Immersion oil )
3 . Reagents
A . Wright’s stain it is prepared as follows
- Weigh 0.2 g of the powder .
- Transfer part of it in a clean dry mortar .
- Add acetone free methanol ( about 25 ml )
- Grind the powder by using a pestle .
- Transfer the ground staining solution to a clean and dry amber colored bottle by filtering through a fillter paper .
- Repeat the procedure till all powdere and totally 100 ml of methanol is used up .
- Store in an amber colored bottle at room temperature ( 25 ° C +_ 5 ° C ) for 1 week standing for about a week
B . Buffer ( pH 7.0 ) It is prepared as follows
- Sodium dihydrogen phosphate = 3 .76 g
- Potassium dihydrogen phosphate = 2 . 10 g
- Distilled water to 1000 ml
Keep at room temperature ( 25 ° C +_ 5 °C ) .
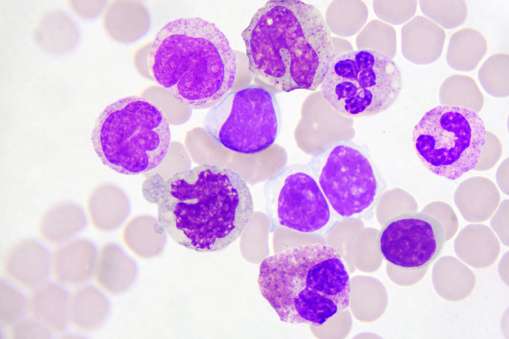
Principle
The polychromic staining solution ( Wright , Leishman , Giemsa ) Contain methylene blue ( basic dye ) and eosin ( acidic dye ) . These basic and acidic dyes induce multiple colors when applied to cells . Methanol acts as fixative and also as a solvent . The fixatve dose not allow any further change in the cells and makes them adhere to the glass slide . The basic component of white cell ( cytoplasm ) is stained by acidic dye ( eosin ) and they are described as eosinophilc or acidophilic . The acidic components ( nuculeus with nucleic acid ) take blue to purple shades by the basic dye ( methylene blue ) and they are called basophilic . The neutral components of the cell are stained by both the dyes .
Procedure
A thin smear is prepared by spreading a small drop of blood evenly on a slide .
Making the film
- Take a clean dry ( grease free ) slide .
- Transfer a small drop of blood near the edge of the slide .
- Place the spreader slide at an angle of 30 ° pull back the spreader until it touches the drop of blood . Let the blood run along edge of the spreader .
- Push the spreader forward to the end of the slide with a smooth movements
- Dry the blood smear at room temperature . Adequate drying is essential to preserve the quality of the film .
Precautions
- Dirty slides do not give an even smear .
- Use an appropriate size of blood drop .
- After putting the drop on the slide , make the smear immediately for even distribution of white blood cells on the slide .
- The thickness of the smear depends on the angle of the spreader . If the angle on than 30 ° , a thicker smear is obtained
- The film must be smooth at the end . There should be no lines extending across or down through the film and it should not contain holes .
Identification marking
By using a lead pencil or a ball pen , write the identification number on the slide .
Fixing the smear
The slide should be stained after marking the smear methanol present in the stain fixes the smear . If the staining is to be done later , the blood smear must be fixed with methanol for 2 to 3 minutes to prevent distortion of cells .
Staining the film
1 . Cover the smear with the staining solution by adding 10 – 15 drops on the smear . Wait exactly for one minute .
2 . Add equal number of the drops of buffer solution . Mix the reaction mixture adequately by blowing on it through a pipette . Wait for 10 minutes .
